Types of Eye Pain
Many patients come to our practice complaining of eye pain – all kinds of eye pain. Some patients describe it as a “needle” going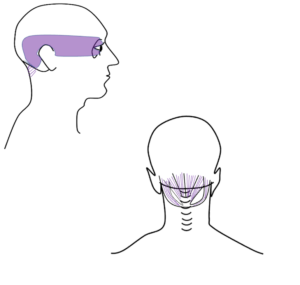 straight through the eyeball to the back of the brain, or perhaps an ache right behind the eyeball, or pressure above the eyebrow. Sometimes the pain is a deep throbbing pain, and sometimes it is hot, searing, radiating pain. The eye pain may occur with reading, computer, or tasks that require a lot of head and eye movements.
straight through the eyeball to the back of the brain, or perhaps an ache right behind the eyeball, or pressure above the eyebrow. Sometimes the pain is a deep throbbing pain, and sometimes it is hot, searing, radiating pain. The eye pain may occur with reading, computer, or tasks that require a lot of head and eye movements.
The first steps to diagnosing the cause of eye pain is to… evaluate the eye. In traumatic brain injury (TBI) the most common eye-related conditions that can cause eye pain is ocular surface inflammation due to dry eye, corneal damage, or inflammation inside the eye. But what if you see your eye doctor and they tell you the eye is TOTALLY normal!? While it might be re-assuring that the eye health is normal, in most cases, this is surprising and frustrating, because… it hurts!
Neck Related Eye Pain
One of the most overlooked etiologies for eye pain post-TBI is the neck. Neck injury or whiplash injury is common in TBI, as the neck absorbs a lot of the shock from the blow to the head. The neck supports and moves the head, but the neck musculature is also intimately associated to supporting eye movements. Don’t believe me? Put your hands on the back of your neck near the base of your skull/on the sides of the spine and move your eyes from the far left to the far right quickly back and forth… did you feel your neck muscles flex?
 When the eyes move quickly from one target to another, they make an eye movement called a saccade, which is a ballistic eye movement that requires a lot of energy and force. The eyes not only have to move as a team accurately from left to right, but the eye muscles must move the eyes against the orbital tissue and fat, requiring a lot of energy. In order for the head to not move with the eyes during this movement, the neck muscles have to engage to keep the head still. So if someone has a neck injury to these supporting muscles, when a patient uses a lot of saccades doing visual tasks like reading or using two computer screen monitors, they are demanding a lot of the neck which can trigger pain.
When the eyes move quickly from one target to another, they make an eye movement called a saccade, which is a ballistic eye movement that requires a lot of energy and force. The eyes not only have to move as a team accurately from left to right, but the eye muscles must move the eyes against the orbital tissue and fat, requiring a lot of energy. In order for the head to not move with the eyes during this movement, the neck muscles have to engage to keep the head still. So if someone has a neck injury to these supporting muscles, when a patient uses a lot of saccades doing visual tasks like reading or using two computer screen monitors, they are demanding a lot of the neck which can trigger pain.
In addition to supporting the head during saccadic eye movements, the neck muscles also engage when the eyes move slowly off axis to reflexively turn the head. Think about how uncomfortable it would be to keep the eyes in a side gaze position when talking to someone next to you, when you could just comfortably turn your head! In fact neuro-muscular studies have found a linear relationship to the muscular engagement activity of the neck and how far you move your eyes to the side – ie the more you move your eyes to the right or left, the stronger the neck muscles contract.1 This cervical-ocular reflex is autonomically controlled, so when patients have neck injuries they may notice that it is easier to read a column of text or on their phone then on a larger screen as the smaller range of motion/field of view for the eyes to roam is less demanding on the neck musculature.
Trigger Points
So how does the neck cause eye pain? The sensory nerves in the neck overlap with some of the trigeminal sensory nerves of the eye. These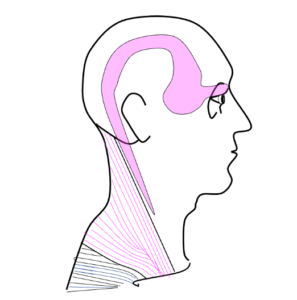 overlapping pain fibers can cause referral patterns – so some patients with neck injury may actually not complain of neck pain at all… but eye pain! These are due to trigger points in the neck muscles – where a problem in one area triggers pain in another area. Common cervical muscles that can refer to the eye include the sternocleidomastoid muscle, upper trapezius, temporalis, suboccipitals, occipito-frontalis, and the splenius cervicis/capitis. How can you tell if your eye pain is neck pain? Well, if you are on the computer or reading and getting eye pain that your eye doctor has already told you is not coming from the eye – try rubbing your neck! If your eye pain improves or worsens with neck palpation, it is likely referred cervicogenic eye pain and you would benefit from evaluation and treatment with an orthopedic physical therapist.
overlapping pain fibers can cause referral patterns – so some patients with neck injury may actually not complain of neck pain at all… but eye pain! These are due to trigger points in the neck muscles – where a problem in one area triggers pain in another area. Common cervical muscles that can refer to the eye include the sternocleidomastoid muscle, upper trapezius, temporalis, suboccipitals, occipito-frontalis, and the splenius cervicis/capitis. How can you tell if your eye pain is neck pain? Well, if you are on the computer or reading and getting eye pain that your eye doctor has already told you is not coming from the eye – try rubbing your neck! If your eye pain improves or worsens with neck palpation, it is likely referred cervicogenic eye pain and you would benefit from evaluation and treatment with an orthopedic physical therapist.
- Bexander CS, Mellor R, Hodges PW. Effect of gaze direction on neck muscle activity during cervical rotation. Exp Brain Res (2005). 167:422-432.
 ABOUT THE AUTHOR
ABOUT THE AUTHOR
Dr. Jacqueline Theis, OD, FAAO is an optometrist with residency training in neuro-optometry, who treats patients with visual complaints and double vision due to brain injury and neurological disease. She has written and lectured international about eye and oculomotor problems after brain injury. You can read more about Dr. Theis HERE.