What is stress hormone? Why do we need it?
Cortisol – “stress hormone” – is made in the adrenal glands, and stimulated by ACTH (adrenocorticotropic hormone) from the pituitary gland. Cortisol goes up in situations of stress (physical or emotional), and is essential in supporting the body such as in times of extreme physical stress.
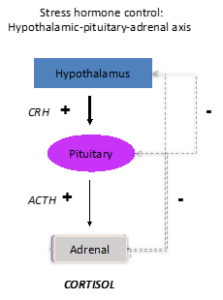
The hypothalamic-pituitary-adrenal system regulates cortisol production. There are disease states that also can lead to too much cortisol (extra cells that make ACTH or cortisol, escaping the normal regulatory feedback loop), or too little cortisol (“adrenal insufficiency,” an inability to increase cortisol secretion when needed, which can happen due to a number of situations including non-cancerous tumors, traumatic brain injury, or the use of cortisol-like glucocorticoids.)
Adrenal insufficiency
Symptoms of adrenal insufficiency may appear as mild fatigue or nausea, or as severe exhaustion, weakness, weight loss, confusion and hypotension. It is important to diagnose adrenal insufficiency – i.e., the inability to make enough cortisol when needed (as distinct from other terms such as adrenal fatigue)—because in adrenal insufficiency, extreme stressors may prompt adrenal crises, which may be fatal if untreated.
There are straightforward ways to diagnose adrenal insufficiency. Cortisol goes up and down naturally over the course of a 24-hr cycle, and is usually highest in the early morning. Thus, a very low serum cortisol in the early morning hours should prompt further evaluation. The “gold standard” test for adrenal insufficiency is a stimulation test in which recombinant ACTH is given, and the body’s ability to secrete cortisol appropriately in response is measured.
If someone is unable to make enough cortisol, replacement is available.
Cortisol excess
There are also ways to diagnose disease states of excess cortisol production, though they are more nuanced, as there are non-disease states that lead to high cortisol levels. Cortisol levels are generally lowest at night, and your doctor might recommend late-night salivary cortisol measurements, or a 24 hour urine collection, as a first measure if there are reasons to suspect a rare disease leading to too much ACTH or cortisol production.
It is important to remember that high cortisol levels are not always indicators of disease—your body may be responding normally to stress, and if you are taking medications —and that there are clear ways to diagnose issues that may affect your health. A neuroendocrinologist may be helpful in this regard.
Using glucocorticoids as a treatment
Glucocorticoids are often used for other medical situations, such as to reduce inflammation, and it’s important to discuss these medications with a doctor evaluating your cortisol levels since glucocorticoid medications will alter cortisol levels and their measurement.
High doses of glucocorticoids taken over time – such as in treatment for other diseases—may lead to the body shutting down its own cortisol production; the body reads excess glucocorticoids as though too much cortisol is being made, and thus can shut down its own cortisol production. When adrenal insufficiency is the body’s natural reaction to high doses of glucocorticoids, and if it is safe to no longer take those glucocorticoids, it is possible to “wake up” the adrenal glands with a slow taper managed by a doctor
For more information, check www.neuroendocrineassociates.com.
 ABOUT THE AUTHOR
ABOUT THE AUTHOR
Tamara L. Wexler, MD, PhD, is an endocrinologist specializing in neuroendocrinology and reproductive endocrinology, nationally recognized for her expertise in post-TBI pituitary dysfunction.