What is Visual Snow?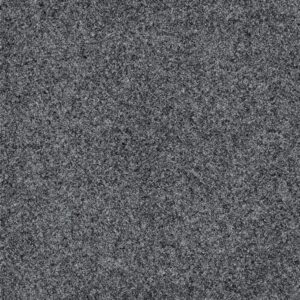
Visual snow is a symptom in which people experience visual disturbances that are described as a flickering of hundreds to thousands of small dots across the person’s entire visual field, and often resembles that of analog television-like static or snow. The dots are often white, black or translucent, although some patients have reported them as colored (rare). This creates a visual experience that’s often unsettling and difficult to ignore, especially when it is acquired or new for a patient (as opposed to being born with it). Visual snow can significantly impact daily life, make concentration challenging, and can flare up depending on certain lighting settings and visual tasks.
 The difference between vitreous floaters and visual snow
The difference between vitreous floaters and visual snow
These small dots are NOT vitreous floaters – which are described as one or a handful of small specks, threads, or cobweb-like shapes that drifts across your field of vision. They often appear as black or gray spots, squiggly lines, or rings that seem to move when you try to look directly at them. Whereas visual snow is always present, doesn’t move with the eyes like vitreous floaters and spans the entire visual field. Vitreous floaters are often caused by age-related changes as the gel liquifies with age and contracts/folds on itself, causing clumps of collagen fibers that cast shadows on the retina, especially when looking at a bright light or uniform background like a clear blue sky or blank piece of paper. While common and usually harmless, a sudden increase in floaters or the appearance of bright flashes of light (like lightening bolts in your vision) can be a sign of a retinal detachment/tear and should be checked ASAP by an eye care professional (optometrist or ophthalmologist) with a dilated eye exam.
The difference between migraine aura and visual snow
Visual snow used to be thought of as an atypical migraine or migraine aura, however, in the past decade visual snow has been defined as a distinct visual disturbance.[i] A migraine aura is a visual disturbance that lasts for about 20-60 minutes that precedes a migraine. Unlike visual snow, the patient may see zigzag lines (aka scintillating scotoma), blind spots, sparkles, stars, or have peripheral vision loss. These symptoms go away for patients often when the migraine starts as occurs in typical migraine aura, or sometimes go away without a migraine which is referred sometimes as an ocular/ophthalmic/retinal or acephalgic migraine – where a patient has a migraine aura but never gets pain/headache. It is not uncommon for patients with visual snow to also suffer from headaches and/or migraines, but the visual snow is a persistent symptom that is unrelated to the migraine itself.
What is Visual Snow Syndrome (VSS)?
Visual Snow Syndrome (VSS) is diagnosed when a patient has had persistent visual snow for longer than 3 months AND has at least two other primary visual symptoms including:[ii]
- Photophobia (light sensitivity)
- Nyctalopia (difficulty seeing in low light or dark environments)
- Palinopsia (persistent after images or perception of a smear or trail of a moving object)
- Enhanced entoptic phenomenon
- Blue-field entoptic phenomenon
- Moving colors in vision
- Persistent afterimages
And may also have some secondary visual and/or non-visual symptoms like
- Tinnitus (ringing in the ears)
- Photopsias (white sparkles/lights)
- Migraine
- Hyperacusis/phonophobia (hypersensitivity to sound)
- Balance disturbances
- Tremor
People with visual snow might experience these other symptoms constantly or intermittently. For some, visual snow can be mildly distracting; for others, it can have a major impact on quality of life.
What causes visual snow?
Some people are born with or have had visual snow since childhood (and cannot recall a time earlier in life that it was not present), this is known as primary visual snow. Whereas other people acquire it later in life, known as secondary visual snow. Review of the literature shows that there are a lot of inciting events or possible contributing comorbidities including but not limited to head/brain injury, post-infection (including gastrointestinal, systemic flu, and upper respiratory infections), increased intracranial pressure, ocular abnormalities (although these are case reports of various retinal and corneal disorders and not a specific type of ocular abnormality that is associated with visual snow), increased/chronic persistent headaches/migraines, alcohol consumption or hallucinogenic use including cannabis and cocaine, as well as some medications. Co-morbid conditions that can occur with VSS include migraine, anxiety, depression, POTS, dizziness, and fibromyalgia.[iii]
Symptoms can be exacerbated (for some but not all patients) by stress, marijuana, caffeine, lack of sleep, increased headache or neck pain and for some patients antidepressant and migraine medications make it worse, while for others it makes their symptoms better.
VSS is a diagnosis based on subjective symptom description and there is no objective test for VSS. Often times numerous tests will be done including but not limited to ocular imaging (OCT), visual field testing, neuroimaging (MRI/CT/PET scans), electrodiagnostics (EEG) to rule out possible physical comorbidities like epilepsy or ocular pathology, but most often ophthalmic and neurologic examination is normal. This is frustrating for patient and provider alike.
We still do not understand what specifically and pathophysiologically causes visual snow – there have been numerous hypotheses in the scientific literature but nothing proven as of yet. In general it is considered a central (brain-related) visual processing disorder due to hyperexcitability of the occipital cortex.[iv]
According to Dr. Theis, who sees a few cases of visual snow in her clinic a month, “Visual snow is probably not one thing, which is why everyone has struggled to find the “one” pathophysiological pathway underlying the symptom. If you read the literature and case reports the causes of visual snow are vast and diverse. Visual snow is likely a general neurologic symptom, like headache, that has numerous etiologies and descriptors and therefore, the only way to treat visual snow, like headache, is to treat the symptom generator. If you find a provider who says they can treat all types of visual snow – be suspicious – because there is not one single cause or treatment for VSS. Trying to treat VSS can be tricky, especially if a patient has multiple comorbidities like they do post-concussion where they have post-traumatic headache, migraine, anxiety, depression, oculomotor dysfunction, and neck pain, and may require a multi-disciplinary team and attempts of various treatment options for an individual.”
How Does Visual Snow Relate to Concussion?
Visual snow can appear after a concussion or other types of head trauma, often within days or weeks of the injury (Mehta 2021). Concussions can disrupt visual processing in the brain, particularly in the areas responsible for integrating and interpreting visual information. The brain’s visual processing pathways are intricate and involve multiple regions, including the occipital lobe, which interprets basic visual input, and other areas involved in eye movements, focus, and light sensitivity. A concussion disrupts the communication between these areas, which can lead to a range of visual issues, including visual snow.
In cases where visual snow appears following a concussion, the symptoms are often part of a broader set of visual or neurological disturbances. Post-concussion patients frequently experience symptoms like dizziness, headaches, and light sensitivity, which can further intensify visual snow, making it challenging for the brain to process visual information normally.
Treating and Living with Visual Snow
For those dealing with visual snow following a concussion, the symptoms can be frustrating and disruptive, but there are strategies to help manage it:
- Orthoptics Visual Therapy: If the underlying cause is related to oculomotor dysfunction, and a patient has objective oculomotor dysfunction on neuro-optometric examination, then working with a neuro-optometrist on eye movement exercises for some patients can provide relief, especially for the palinopsia symptoms, which is thought to be due to abnormal smooth pursuits and/or saccades.[v] Vision therapy can improve coordination between the eyes and the brain, reduce symptoms of visual snow, and address related post-concussion visual issues like dizziness/nausea/headaches with reading and computer use.
- Reduce Screen Time and Blue Light Exposure: Screens and intense blue light sources like fluorescent lights can
 exacerbate visual snow for some people. Reducing screen time or using blue light filters on devices can ease visual fatigue and minimize visual snow. The most helpful tint for visual snow, especially for patients with co-morbid migraine is FL-41 – but patient beware, not all FL-41 filters are the same, as Dr. Theis found out in her research looking at the spectrophotometry of FL-41 filters.[vi] So some may be better suited for a patient than others – and the cost of the lenses are not always associated with the effectiveness of the lens. At Virginia Neuro-Optometry, Dr. Theis has acquired a variety of FL-41 filters for patients to try to see if any one of them works. She also has some blue filters which in the literature has been reported to be effective, but she has found this not always to be the case.
exacerbate visual snow for some people. Reducing screen time or using blue light filters on devices can ease visual fatigue and minimize visual snow. The most helpful tint for visual snow, especially for patients with co-morbid migraine is FL-41 – but patient beware, not all FL-41 filters are the same, as Dr. Theis found out in her research looking at the spectrophotometry of FL-41 filters.[vi] So some may be better suited for a patient than others – and the cost of the lenses are not always associated with the effectiveness of the lens. At Virginia Neuro-Optometry, Dr. Theis has acquired a variety of FL-41 filters for patients to try to see if any one of them works. She also has some blue filters which in the literature has been reported to be effective, but she has found this not always to be the case. - Physical Therapy – If the visual snow symptoms are worse in certain head postures or with neck pain in a patient with a whiplash injury, then addressing the neck with orthopedic physical therapy may improve VS symptoms.
- Reducing Stress, Decreasing caffeine/alcohol intake, Increasing Sleep, and Managing Mental Health – since stress, alcohol, caffeine, lack of sleep and anxiety/depression are linked to visual snow, then addressing these comorbidities may help.
- Medication: In some cases, medications prescribed by a medical doctor (neurologist, physiatrist, etc) may help alleviate symptoms of visual snow, especially if it’s accompanied by migraines. However, this approach is often individualized based on a patient’s unique needs and symptoms and there is no single medication or supplement that is proven to treat VS.
- Supplements: for patients with photophobia or glare sensitivity or reductions in night vision – some supplements like lutein/zeaxanthin, turmeric, and omega 3s, may be helpful – as they have shown to help improve contrast sensitivity and glare/light sensitivity in some patients. It can take 6-12 months to notice changes, and not all supplements are the same and there is no single supplement that is proven to be effective for visual snow.
The Road to Recovery
For many people, visual snow following a concussion is temporary and resolves as the brain heals. However, recovery from TBI is different for everyone, and some may experience lingering symptoms. The key to managing visual snow and related post-concussion symptoms is a combination of time, patience, support and targeted rehabilitation from specialists in neuro-optometry, neurology, and rehabilitation (PT/OT).
While there’s still much to learn about the relationship between visual snow and concussion, advances in neuro-optometric research continue to shed light on how the brain processes visual information and how these processes are affected by trauma. Through personalized treatment and support, many individuals can find relief from symptoms and reclaim their quality of life.
If you’re experiencing visual snow or other vision disturbances after a concussion, consider consulting a neuro-optometrist or healthcare provider who specializes in TBI. With the right resources and care, relief and recovery are within reach.
[i] Schankin CJ, Maniyar FH, Digre KB, Goadsby PJ. ‘Visual snow’ – a disorder distinct from persistent migraine aura. Brain. 2014 May;137(Pt 5):1419-28. doi: 10.1093/brain/awu050. Epub 2014 Mar 18. PMID: 24645145.
[ii] Ciuffreda KJ, Han ME, Tannen B, Rutner D. Visual snow syndrome: evolving neuro-optometric considerations in concussion/mild traumatic brain injury. Concussion. 2021 Apr 9;6(2):CNC89. doi: 10.2217/cnc-2021-0003. PMID: 34084555; PMCID: PMC8162163.
[iii] Mehta DG, Garza I, Robertson CE. Two hundred and forty-eight cases of visual snow: A review of potential inciting events and contributing comorbidities. Cephalalgia. 2021 Aug;41(9):1015-1026. doi: 10.1177/0333102421996355. Epub 2021 Feb 20. PMID: 33615842.
[iv] Traber GL, Piccirelli M, Michels L. Visual snow syndrome: a review on diagnosis, pathophysiology, and treatment. Curr Opin Neurol. 2020 Feb;33(1):74-78. doi: 10.1097/WCO.0000000000000768. PMID: 31714263.
[v] Ciuffreda KJ, Han ME, Tannen B, Rutner D. Visual snow syndrome: evolving neuro-optometric considerations in concussion/mild traumatic brain injury. Concussion. 2021 Apr 9;6(2):CNC89. doi: 10.2217/cnc-2021-0003. PMID: 34084555; PMCID: PMC8162163.
[vi] Theis J, Stern J. Spectrophotometric evaluation of light sources that trigger photophobia in patients with brain injury and the Corresponding reduction with tinted lenses and/or environmental adaptations for indoors, outdoors, and electronic devices. North American Brain Injury Society – American Brain Injury Conference. 2024 Poster Abstract #42. Las Vegas, NV.